
Chronic Obstructive Pulmonary Disease (COPD) is an umbrella term for two lung conditions that cause the lungs to become inflamed and damaged, resulting in breathing difficulties.
It affects around 1.2 million people in the UK, and according to the World Health Organisation (WHO), it is the 7th leading cause of poor health worldwide and the 3rd leading cause of death in 2019.
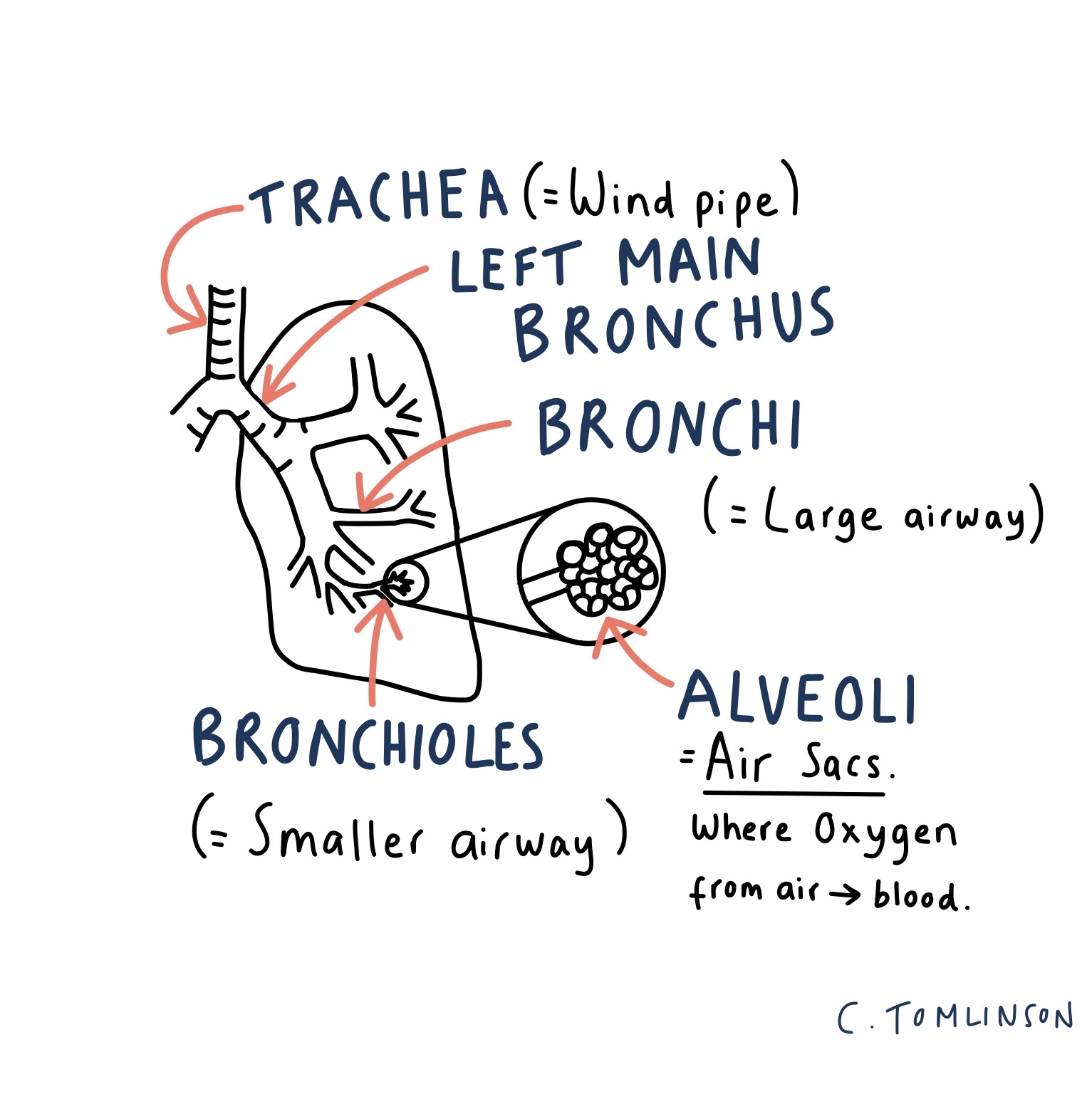
The two conditions that make up COPD are:
- Chronic bronchitis – inflammation of the airways over a long period. Lots of mucous is produced in the airways, making it harder to breathe.
- Emphysema – where the air sacs (alveoli) in the lungs become damaged, so it’s harder for oxygen in the air to get into the blood.
Contents:
- Risk factors
- Signs and symptoms
- When should you see your GP?
- How will your healthcare practitioner diagnose COPD?
- How can COPD be treated?
- Psychological impact of COPD
- In summary
What Increases The Risk of COPD?

- Smoking – this is the leading cause of COPD; 20% of smokers develop the disease, and 90% of people who are diagnosed are smokers or ex-smokers.
- The risk increases with the amount smoked daily and the duration of smoking. Passive smoking – being exposed to smoke from others – also contributes to risk.
- Smoking increases the risk as the chemicals inhaled are toxic and carcinogenic (increase the risk of cancer); this irritates and damages the lungs.
2. Age – it typically affects older adults, as it develops gradually over time.
3. Recurrent chest infections as a child increases susceptibility, as it increases the risk of chronic bronchitis (one of the two conditions that make up COPD).
4. Environmental factors – Air pollution and long-term exposure to different chemicals/dust/fumes through work increase risk. This is because pollutants can cause inflammation in the lungs, and damage DNA in cells causing epigenetic changes that play role in increasing COPD risk.
- An epigenetic change is where environmental factors affect our DNA, which in turn can affect how essential proteins work in the body (proteins that are needed for our cells to function).
5. Genetics
- Alpha-1 antitrypsin deficiency is a genetic condition (passed down from your parents) that affects the body’s ability to produce a protein called Alpha-1, which protects the lungs. Without this protein, the air sacs (alveoli) are damaged, leading to emphysema. You may be tested for this if you’re diagnosed with COPD under the age of 40, or if it runs in your family.
Vaping – we don’t know much about the long-term affects of vaping on our health yet, but it is a growing concern considering how popular it is (3.2 million adults in England currently vape, 18% of which are 18-year-olds). A 2016 study in mice suggested that vaping nicotine-based products triggered lung inflammation and damage which are associated with COPD; given that COPD tends to affect older adults, though, it may be several years before we have definitive evidence whether there is an association between the two.
What Are The Signs and Symptoms?
Common signs and symptoms include:
- A persistent chesty cough with significant phlegm production.
- Breathlessness, especially during physical exertion.
- Wheezing – a noisy whistling/rattling sound when breathing that may be audible or only heard through a stethoscope.
- Increased susceptibility to chest infections.
Symptoms will slowly worsen over time and cannot be cured, but treatment can help slow down the progression.
Exacerbations – sudden worsening of symptoms over the course of a few hours to days – can occur and are often triggered by chest infections or by environmental factors like smoking or air pollution. During an exacerbation you may cough more frequently, notice changes in phlegm colour (commonly yellow or green) and feel more breathless.
When Should You See Your GP?
Consult your GP if you have any of the above symptoms, particularly if you smoke (or used to smoke) and are over 35 years old. Your GP will ask about your symptoms, other health conditions, family medical history, and smoking status.
How Will Your Healthcare Practitioner Diagnose COPD?
Diagnosis usually involves being referred for a breathing test called Spirometry. This is where you breathe into a device that measures airflow.
Additional tests may include:
- A chest X-ray to rule out other causes of your symptoms.
- A blood test to check for an infection or other issues.
- A sputum sample – if you’re coughing up green or yellow phlegm, a sample may be sent off to check for infection.
How Can COPD Be Treated?
One of the most important things to do after diagnosis is to stop smoking, as this is the only proven way to slow down disease progression.
Your Doctor can help you through offering nicotine replacement therapy and referring you to the NHS stop smoking service for further support.
To find out more about NHS stop smoking services, use this link:
https://www.nhs.uk/live-well/quit-smoking/nhs-stop-smoking-services-help-you-quit/

You will be offered a one-off pneumococcal vaccine and yearly influenza vaccine, to reduce the risk of severe chest infections.
Medical Management:
- Inhalers (e.g., Salbutamol) – help to open airways, and can be used when exercising to improve exercise tolerance.
- The same medications may be given via a nebuliser if symptoms are still severe despite maximum treatment with inhalers.
- A nebuliser is a device that turns the medication into a fine mist that can breathed in. You will likely be seen by a respiratory specialist first before being prescribed nebulisers.

- Mucolytics (e.g., Carbocysteine) – a medication that helps to break up phlegm.
- This may be given if you have a long-term cough and are regularly coughing up phlegm.
- Steroids (e.g., Prednisolone) – used during an exacerbation to reduce airway inflammation.
- Antibiotics – prescribed for chest infections causing an exacerbation.
- They may be prescribed long-term if you don’t smoke and you keep having frequent exacerbations.

- Long term Oxygen therapy – initiated by specialists for severe cases where your blood oxygen levels are low.
- This option is only available to non-smokers due to fire risks.
- Lung surgery or lung transplant – this is only considered in severe disease after seeing a specialist, and is only an option for a small number of patients.
If your symptoms get worse and you think you’re having an exacerbation, you should see your Doctor promptly; you may need antibiotics, steroids, and may need treatment in hospital.
Regular check-ups with your Doctor are recommended at least once a year (for a review of your symptoms and medications) and after every exacerbation.
The Importance of Physical Activity In COPD
Regular exercise is essential for people with COPD. While it can’t reverse the condition, it can significantly improve your breathing and overall well-being.
Many people find exercise challenging with COPD due to breathlessness, which can create a cycle of anxiety, reduced activity and increased symptoms.
Feeling more breathless during exertion is normal, though; however, individuals with COPD may experience this response more quickly as their lungs are having to work that bit harder.
Your body can also become “de-conditioned” – the less exercise you do, the less able you are to do it, as the muscles that are used for certain activities become weaker. That’s why when you do start exercising, it’s important to start slowly and gradually increase intensity.

Before starting an exercise program, it is important to consult your Doctor for personalised advice tailored to your specific circumstances. It is also advisable to have someone with you during exercise sessions in case you feel unwell.
There are different types of exercise that are important in COPD:
- Aerobic exercises – work your heart and lungs to improve endurance, for example, walking, riding a bike or swimming.
- Strengthening exercises – help increase the strength of your muscles, including your breathing muscles. Options include free weights, bodyweight, resistance bands, or weightlifting equipment.
- Strengthening exercises can be adapted to be done whilst sat down if needed too; follow this link for more: https://www.nhsinform.scot/illnesses-and-conditions/lungs-and-airways/copd/exercising-with-copd/
- Breathing exercises – help increase the strength of your breathing muscles, which will make it easier to breathe with less effort in time.
- One example is Pursed Lip Breathing –breathe in through your nose for around 2 seconds, purse your lips (as if you’re whistling or about to blow out candles), then breathe out very slowly for around 4-6 seconds. There are other techniques too, but they can be trickier to do, so it is best to be taught these by a respiratory therapist or healthcare practitioner.
If you start having pain in your chest, arm, neck or jaw, feel dizzy or light-headed, feel sick or weak, then stop exercising and sit down. If you don’t feel better after doing so, seek immediate medical attention.
Lifestyle Modifications (Beyond Exercise)
It’s vital to maintain a healthy weight with COPD; being overweight can exacerbate breathlessness while unintentional weight loss (which can be common in COPD) can make your muscles weaker, including the muscles that help you breathe. It’s important to eat a healthy and balanced diet as a rule (and the NHS Eatwell Guide is a good reference point for this), but nutritional requirements in COPD should be considered on a person to person basis, as energy requirements may be higher than other people’s. Speak to your Doctor or Dietitian about this for more information.
Before leaving home, have a look at the weather forecast as many people find their symptoms are worse in the cold weather or drier conditions. Being around smoke, fumes, or dusty places can also exacerbate symptoms.
You may not be able to fly on an airline depending on the severity of your condition, so you should see your Doctor before flying. You may need a pre-flight assessment, and an airline can refuse to take you if they’re concerned for your safety.
If you drive, you don’t need to notify the DVLA unless you have any of the following: fainting associated with coughing, severe dizziness, blackouts. If in doubt about whether you can drive, discuss this with your Doctor. Do not drive if you do not feel safe to do so.
Financial Support
People with COPD may find that their symptoms make it very difficult to work. If you have a job but are unable to work because of your illness, then you’re entitled to Statutory Sick Pay (£116.75 per week). If you don’t have a job and cannot work due to your illness, you may be entitled to Employment and Support Allowance. If you are caring for someone with COPD, you may be entitled to Carer’s Allowance (£81.90 per week).
What Other Services Are There To Support You If You Have COPD?
If your symptoms are significantly impacting your life, or you’ve recently been in hospital for an exacerbation, you may be referred for pulmonary rehabilitation. This is an individually tailored education and exercise program, that helps people better understand and manage their symptoms.
You may be referred to a physiotherapist if you’re coughing up a lot of phlegm, to learn breathing techniques which can help you clear your chest, or to learn how to use positive expiratory pressure devices.
- These devices allow air to flow in freely when you breathe in, but not when you breathe out – this means when you breathe out you have to breathe harder against resistance, helping air get behind the phlegm and move it away from the lungs (so it can be coughed up) and helping keep airways open.
Psychological Impact of Living With COPD
COPD can have a big impact on your mood; studies have shown that rates of both anxiety and depression are higher in people with COPD.
Suffering from anxiety can also affect you physically; if you have a panic attack where intense feelings of panic or worry come on quickly, it can affect your breathing. Sometimes the symptoms of COPD can trigger these feelings too, which makes symptoms worse. If this happens, it’s important to try and slow your breathing. One way to do this is by deep breathing – breathing in slowly through your nose, and out through your mouth.
Talk to your healthcare practitioner early about your mood, as there are lots of ways they can help – from discussing different coping strategies, to referring you to a mental health practitioner for further support.
Consider joining support groups where individuals share similar experiences, for example, Asthma + Lung UK – a UK-based charity that runs a monthly support meeting for people with COPD.
If you have COPD and are struggling with your mental health, see the links below for more support:
https://copdandme.co.uk/emotional-wellbeing/emotional-impact-of-copd/
https://www.asthmaandlung.org.uk/living-with/mental-health/anxiety
https://www.asthmaandlung.org.uk/living-with/mental-health/depression
To Summarise:
COPD is a common lung condition affecting 1.2 million people in the UK, and the biggest risk factor is smoking.
While there is no cure, early diagnosis and proactive management can significantly improve quality of life; embracing a healthier lifestyle by quitting smoking, eating well and exercising regularly are all crucial steps towards better lung health.
If you have COPD yourself or know/care for someone with COPD, I’d love to hear your personal experience if you feel comfortable sharing. Equally, if you’re a healthcare practitioner who has cared for people with COPD, I’d love to hear your thoughts and insights too. Please leave a comment down below!
references:
Most sources are hyper-linked in the text above. See below for sources used for general information.
https://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/living-with/
https://www.copdfoundation.org/Learn-More/I-am-New-to-COPD/Breathing-Techniques.aspx
https://www.webmd.com/lung/copd/copd-and-exercise-breathing-and-exercise-programs-for-copd
https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)

Leave a comment