The National Health Service (NHS) is an immense system; it is the biggest employer in Europe, with over 1.3 million staff in total. Within it are hundreds of organisations of varying sizes, each with their own roles and responsibilities. It can be hard enough as it is for people working within the system to navigate the NHS as trusts often have slightly different ways of doing things and different services on offer – it comes as no surprise therefore that, as a patient, it can be difficult to work out who you need to see and who is responsible for what.
Recent evidence supports this, suggesting there is confusion amongst the public about which NHS service to use and when; in 2014, self-treatable conditions accounted for 19.1% of Accident & Emergency (A&E) attendances, which equates to £290 million in working time and healthcare costs. A study looking at first time A&E attendances across 13 acute trusts in 2011-2014 found that 15.1% of cases were “non-urgent” and could have been addressed by alternate care services.

Understanding how to navigate this complex system is crucial; since the NHS was founded in 1948, it has upheld the principle of providing healthcare that is “free at the point of delivery”, a trait that sets it apart from many other healthcare services across the globe. Knowing when and how to use different NHS services is vital for the NHS to run efficiently, allowing it to continue providing free healthcare for everyone, and to ensure patients receive appropriate care improving the healthcare experience for everyone involved.
This guide aims to demystify the services the NHS offers, providing you with essential information on what is available to you and how to access the care you need.
Contents.
- What to do if I have a general health concern or query?
- I’m struggling to get a GP appointment, is there anyone else I can see?
- What to do if I need health advice ASAP, but my GP is closed, and it isn’t a medical emergency?
- What to do if I know I need urgent treatment, but it isn’t a medical emergency?
- What to do in a medical emergency?
- I need to speak to someone about sexual health – what should I do?
- When should I see my dentist?
- I’ve had a change in my eyesight – what should I do?
- I’m really struggling with my mental health, what should I do?
- In summary.
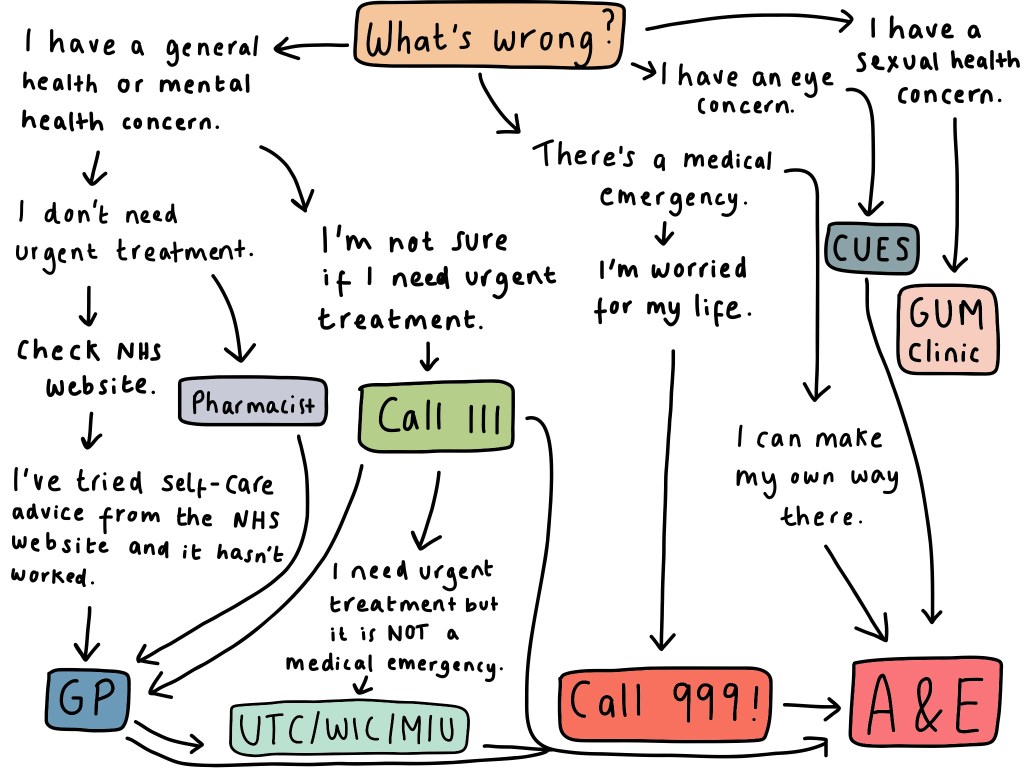
- Flowchart summarising how to access healthcare services in the UK.
What To Do If I Have a General Health Concern or Query?
For general advice, the NHS website has a wealth of information available on self-care for common health conditions. If symptoms persist after a few days despite self-care, or if it is reoccurring, then you should seek medical attention.
GP surgeries serve as the first point of contact for NHS patients seeking general healthcare. These practices house a team of healthcare practitioners (HCPs), each contributing a unique skill set to provide comprehensive patient care, and may include GPs, Nurses, Health Care Assistants, Community Paramedics, Pharmacists, and Physicians Associates.
Healthcare Practitioners (HCPs) working in this setting are experienced in treating chronic health conditions and common medical conditions, as well as advising on whether patients need to attend A&E and referring onto specialist services as needed.
When you contact your GP practice, an appointment will be made with a HCP that is best suited to meet your needs. Depending on your practice, appointments may be made by phone, website, or by attending the reception. Urgent cases will be seen the same day; if you think your issue is urgent, it is important to inform the practice when you make the appointment.
Conditions that can be assessed and managed by your GP include:
- Headaches – migraines, cluster headaches, medication overuse headaches, tension-type headaches.
- Chronic pain.
- Tiredness.
- Unexplained weight loss.
- Persistent cough >3 weeks.
- Yellowing of the skin.
- A new mole, or one that is growing/has changed in colour.
- Change in bowel habit.
- Mental health conditions.
- Chronic (long-term) health conditions – including diabetes, hypertension (high blood pressure), asthma, COPD.
- Arthritis.
- Dementia.
- Worsening and persistent ear pain/sore throat.
- Unexplained rashes.
- Menopause management.
I’m Struggling To Get a GP Appointment – Is There Anyone Else I Can See?
Prescribing Pharmacists can now advise and prescribe prescription-only medications for the following medical conditions, without you needing to see a GP: sore throat (5 years old +), earache (1 year – 17 years old), infected insect bites (1 year old +), uncomplicated urine infections in women (16-64 years old), sinusitis (12 years old +), impetigo and shingles (18 years +), and advise on emergency contraception. You can also go to a Pharmacist for blood pressure checks.
What To Do If I Need Health Advice ASAP, But My GP Is Closed, and It Isn’t a Medical Emergency?
NHS 111 is a 24/7 helpline which offers health advice, helping people get the right treatment. Call 111 if you feel you need health advice or urgent care but your GP/pharmacy/dental practice are closed and it can’t wait until tomorrow, if you’re not sure if you need urgent care, or if you think you need urgent care but are not sure which service to use.
NHS 111 can assess your symptoms over the phone, provide medical advice, and direct you to the most appropriate healthcare service. They can also book you into urgent care services e.g., urgent treatment centre if needed, or arrange a call-back from a HCP e.g. the out-of-hours GP.
What To Do If I Know I Need Urgent Treatment, But It Isn’t a Medical Emergency?
If a condition needs urgent medical treatment but isn’t life-threatening, an urgent care centre should be attended. Urgent care centres include walk-in centres (WICs), urgent treatment centres (UTCs) and minor injuries units (MIUs); the aim of urgent care centres is to be a locally accessible alternative to A&E.
WICs are healthcare facilities that provide medical care for minor injuries and illnesses, and you don’t need an appointment to attend. Walk-in centres are typically Nurse led. They can provide treatment for:
- Rashes.
- Coughs, colds, and flu-like symptoms.
- Earache and sore throats.
- Water infections.
- Cuts and bruises.
- Stomach bugs.
- Minor burns.
- Sprains and strains.
- Emergency contraception.
- Insect and animal bites.
- Women’s health e.g., thrush.
UTCs are for people needing urgent medical attention that isn’t life threatening. They are like walk-in centres, but have access to more diagnostic tests including X-rays, and can see both walk-ins and booked in patients (who have been booked in by NHS 111). They tend to be GP led, are open for at least 12 hours a day every day of the year and have clear referral pathways into A&E departments should patients need it. If in doubt whether you should attend a WIC or UTC, call 111 beforehand.
MIUs offer advice and treatment for a variety of minor injuries including strains, minor burns, grazes/wounds that may require stitching, wounds. They do not typically treat minor illnesses. They tend to be led by experienced nurses or emergency nurse practitioners (ENPs – who have training in emergency care).
What To Do In a Medical Emergency?
A medical emergency is a serious medical illness or injury that requires immediate medical attention.
If you feel this could be life-threatening or result in permanent disability if not treated, you must call 999 and ask for the ambulance service. An ambulance will be sent out to you, and any potentially life-saving treatment needed can be given in a pre-hospital setting.

If there is a medical emergency but it isn’t immediately life-threatening and you can get to A&E safely, then you must do so, and you do not need to call 999. Please do not drive if you feel unable to do so.
A&E is an emergency service which is open 24 hours a day, 365 days a year. Practitioners who work there are highly trained in emergency medicine and can deliver life-saving interventions quickly; they are not experienced in treating chronic health conditions or minor ailments.
On arrival you will be seen promptly by the triage team who conduct an initial assessment to determine the urgency of treatment – you will then be streamlined to a certain department within A&E.
This can include Resus (very unwell patients who require significant life-saving interventions), Majors (for acutely unwell patients), Minors (for minor injuries). Some hospitals may have an ambulatory assessment unit for patients referred by GPs or urgent care centres – these units are for patients who are able to walk (hence “ambulatory”), sit, and wait for further investigations. Patients can be moved between areas if they become more unwell.
When you attend the department, you need to be prepared to wait – waiting times can be upwards of several hours and patients are seen based on the severity of their condition, not arrival time. Arriving by ambulance will not give you priority over walk-in patients either, as everyone attending the department is assessed by the triage team on arrival.
The list of medical emergencies is not exhaustive, but this list covers the main conditions that would be an appropriate use of calling ‘999’ (as can be immediately life-threatening):
| Condition | Presentation |
| Cardiac arrest | Where someone isn’t breathing and there is no pulse. CPR needs to be started if first aid trained. |
| Anaphylaxis | A severe allergic reaction that develops rapidly. Symptoms include swelling of the throat/tongue/lips, itchy skin, a red raised rash (hives, known medically as wheals), difficulty breathing, dizziness, pale skin. |
| Major trauma | Including road traffic accidents (RTAs), or a fall from height. Often present with multiple serious injuries. |
| Loss of consciousness | Where someone is still breathing and has a pulse, but they’re not responding to you. |
| Severe bleeding | Bleeding that still won’t stop after heavy pressure is applied. |
| Suspected heart attack/severe chest pain | Classically described as feeling like an “elephant is sat on the chest”. Presents with chest pain that may spread into the left arm or jaw, often associated with looking pale/sweaty/clammy and shortness of breath. |
| Suspected stroke | Sudden onset of weakness in one side of the body, slurred speech, facial droop. |
| Severe breathlessness | Breathing very fast, unable to talk in full sentences. |
| Severe burns | Injury to the skin due to heat, electricity, chemicals, or radiation. |
| Uncontrollable seizures (fits) | Including seizures in known epileptics that aren’t responding to usual treatments (status epilepticus – seizure lasts >5 minutes, or multiple seizures back-to-back without regaining consciousness). There are different types of seizures, the most common is a tonic-clonic seizure which involves rhythmic jerking of the limbs. |
| Hypoglycaemia | Where blood sugar drops very low, most common in type 1 diabetics and people who take insulin. Symptoms can include dizziness, anxiousness, sweating/shaking, tingling lips/cheek/tongue, palpitations, confusion, and loss of consciousness. |
| Hypothermia | Where body temperature drops very low. Signs and symptoms include cold and pale skin, confusion, weakness, slowed heart rate and breathing. |
| Drowning | This can affect breathing, can cause confusion, tiredness, pale skin, and lead to cardiac arrest. |
| Spinal cord compression | Sudden onset back pain associated with urinary/faecal incontinence, saddle anaesthesia (reduced or altered sensation in the area of the body that would touch a saddle if sitting on one) and shooting pains down both legs. |
| Severe head injury | If following the head injury there are any neurological symptoms (weakness in their arms/legs, sensory changes, severe neck pain, seizures, unable to walk or speak etc). |
The following are medical emergencies too, but these may not be immediately life-threatening – depending on individual circumstances you may be able to make your own way to A+E:
| Condition | Presentation |
| Sudden onset confusion | When someone isn’t orientated to time, place, or person. |
| Sudden onset severe abdominal pain | Especially if worsening and not alleviated with pain relief, if the patient has had recent abdominal surgery, is vomiting, isn’t opening their bowels/passing wind, or their abdomen is distended. |
| A severe head injury | Where there has been a loss of consciousness, persistent headache since that isn’t relieved by painkillers, vomiting, confusion, memory loss, blood/clear fluid from nose or ears, bruising behind ears or around eyes, or on blood thinners. Note if you have had a severe head injury yourself you MUST NOT drive. |
| Persistent nosebleed | A nosebleed that doesn’t stop after firm pressure is applied to the soft part of your nose for 20 mins. |
| Poisoning or drug overdose. | Taking more than is recommended of a substance, whether it is a prescription, over-the-counter medication, legal or illegal drugs. Includes household products that are not for ingestion too. |
| Sudden severe headache. | Especially if the pain reaches its peak within 60 seconds, and is associated with confusion, nausea/vomiting, trouble speaking, seizures. |
| Severe infections | High fevers that aren’t coming down with paracetamol, fast breathing/heart rate, pale and clammy skin, confusion, if associated with headache and a stiff neck, or a red/swollen/painful joint. |
| Persistent severe vomiting or diarrhoea | Especially if there are signs of clinical dehydration – sunken eyes, headache, reduced urine output, rapid heartbeat/breathing. |
| Suicidal thoughts or behaviours | Thoughts of wanting to end your life or making plans to do so. |
| Sudden blindness | Especially if a sudden change in your vision, or associated with a painful red eye/trauma to the eye. |
I Need To Speak To Someone About Sexual Health – What Should I Do?
Genitourinary Medicine (GUM) clinics are free and confidential clinics that offer advice and treatment for anything related to sexual health and are available to everyone. Information will not be shared with your GP without your permission. Some clinics may be drop-in, others you may need to book an appointment in advance.
Services they offer include sexually transmitted infection (STI) testing and treatment (including partner notification), human immunodeficiency virus (HIV) testing and support, pre- and post-exposure prophylaxis for HIV, contraception advice, pregnancy testing, counselling services, and support after rape or sexual assault.
You can find your nearest GUM clinic using the NHS website using the following link: https://www.nhs.uk/service-search/sexual-health-services/find-a-sexual-health-clinic/
When Should I See My Dentist?
You should see your dentist for routine dental care and check-ups. If you have toothache, or any problems relating to your gums (including mouth ulcers that don’t heal after 3 weeks’), abscess within your mouth, or any bleeding in your mouth that won’t stop, you should also contact your Dentist, not your Doctor.
I’ve Had a Change In My Eyesight – What Should I Do?
If the change in your eyesight has been gradual, you should book in to see an Optometrist. They can diagnose and treat common vision problems, including glaucoma.
For any other concerns about your eyes or eyesight (especially if acute), you can use the Community Urgent Eye Service (CUES). If you are registered with a GP then you can use this service, and it is for people of all ages. To make an appointment, call one of the participating practices (and there are many across the UK) – you can find them via this link: https://primaryeyecare.co.uk/find-a-practice/
If you have any sudden changes in your vision/an acutely painful red eye/trauma to the eye, and there is no optical practice near to you, then you should attend A&E.

I’m Really Struggling With My Mental Health, What Should I Do?
Generally, the first port of call for concerns related to your mental health is your GP. However, if you feel you are at breaking point and need urgent help, then there are a few options. You need to:
- Call your GP and ask for an emergency appointment, or NHS 111.
- Call the Crisis team if you have their contact number already – this is a community based mental health service that provide a rapid assessment +/- treatment if needed.
- Go to A&E.
- Call 116 123 to talk to Samaritans – a free listening service offering confidential support from trained volunteers.
In Summary:
Bringing it all together; the general process you should follow when choosing to access a healthcare service in the UK is as follows:
This guide provides essential information needed for people to use healthcare services effectively in the UK, empowering you to be proactive in your own care and make informed decisions about your healthcare needs. Understanding what services are available to you not only ensures timely and appropriate care, but also contributes to the functioning of the NHS, allowing it to continue providing healthcare that is free at the point of delivery and available to everyone.
To note – this information is for general guidance and may vary by location or change over time. If you have any questions, please contact your healthcare provider.
References:
https://www.england.nhs.uk/urgent-emergency-care/nhs-111/accessing-nhs-111/
https://www.scottishambulance.com/our-services/emergency-care/when-should-you-call-999/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7460304/
https://www.healthwatch.co.uk/advice-and-information/2024-04-01/what-can-pharmacy-first-scheme-do-me
https://www.nhs.uk/mental-health/

Leave a comment