Let’s talk about contraception: an essential part of reproductive health that can often feel overwhelming when there are lots of options available. How are you supposed to know what’s best for you?
While many contraceptive methods rely on hormones, there are times when avoiding them is preferred or necessary. Whether you’ve experienced side effects, have a medical condition limiting hormonal choices, or simply wish to follow a more natural approach, non-hormonal contraception can still effectively prevent pregnancy when used correctly.
This guide will introduce you to the main non-hormonal methods available, explaining how they work, their effectiveness, and the advantages and disadvantages of each, helping you navigate contraceptive options so you can make an informed choice that suits your unique circumstances.
Rest assured, hormonal options and emergency contraception will be covered in detail soon – but for now, let’s focus on the hormone-free choices.
DISCLAIMER:
Although I am a practising doctor, the information on this site is for educational purposes only. It does not take into account your personal circumstances, which can significantly affect medical decision-making and treatment. This content does not constitute medical advice, and therefore should not be relied upon for diagnosis or treatment. Always seek the advice of a qualified healthcare provider regarding any medical concerns. Any actions you take based on information from this site are at your own risk.
Back-to-basics: How Does Pregnancy Start?
Before we get into the main part of the article, let’s have a look at how pregnancy starts, so we can better understand how it can be prevented by contraception.
Pregnancy starts when a sperm cell from semen meets a fertilised egg released from the ovary during ovulation. The fertilised egg travels to the uterus and implants into its lining, and the pregnancy begins.
Many non-hormonal contraceptive methods act to prevent the sperm cell from fertilising an egg cell.
Contents
- Fertility awareness methods
- Lactational amenorrhoea
- Withdrawal method
- Barrier methods
- Sterilisation
- In summary
- Further resources
Fertility Awareness Methods (FAMs)
This method involves tracking specific signs throughout your menstrual cycle to identify fertile days – the time when pregnancy is most likely. Fertility peaks around ovulation, the day that an egg is released from the ovaries.
There are 3 main indicators, and ideally you should track all of them to increase the success rate. When used altogether, this is known as the symptothermal method:
- Basal body temperature:
- Taken in the morning as soon as you wake up, ideally using a reliable digital or rectal thermometer.
- Your temperature rises by around 0.4 degrees when you ovulate. Tracking the trend over a few months can help give you an idea of when you are most fertile.
- You should use alternate contraception in the days around ovulation. With this method, the “safe days” where you can have unprotected sex begin three days after the temperature rise, and end when your temperature drops again before your next period.
- Note: Lifestyle factors such a stress, drinking alcohol, being sick, or smoking, can all have an effect on your temperature, though.
- Consistency and colour of cervical mucous.
- Around ovulation, your discharge tends to be clear, slippery, stretchy, and more abundant. This tends to last for around 4 days, and are “unsafe days” for unprotected sex.
- After ovulation, mucus thickens, becomes cloudy and sticky, and there is less of it – this signals the “safe” period, which lasts for around 11-14 days until your next period.
- Note: Lots of factors like having sex, using lubricants, having a sexually transmitted infection, can all affect your discharge.
- Cycle charting.
- Tracking your period over several months can help you predict the days in your cycle that you’re most likely to be fertile. Click here for the full method from Planned Parenthood.
- You should ideally track at least 6 periods. If your cycles are shorter than 27 days or if they differ in length, this method is unlikely to be accurate.
| Advantages | Disadvantages |
|---|---|
| No hormones or side effects. | It’s less effective* than other forms of contraception, and is user-dependent (it requires discipline). |
| Suitable for most women (except those with irregular cycles, short cycles, who have recently stopped hormonal contraception, or where pregnancy isn’t advised for medical reasons). | No protection against sexually transmitted diseases (STDs) e.g., Chlamydia. |
| It’s non-invasive. | Often takes several menstrual cycles to learn the technique. |
| Lifestyle factors can affect reliability. | |
| Requires abstinence from sex or alternate contraception during fertile days. |
*24% of women on this method experienced an unintended pregnancy within the first year with typical use, brought down to 1-9% with perfect use**. The risk of pregnancy therefore is higher than most other forms of contraception with typical use.
**Perfect use = following instructions, every time. Typical use = what usually happens in real life.
Lactational Amenorrhoea Method (LAM)
Exclusive breastfeeding following childbirth suppresses ovulation naturally by increasing prolactin levels, which inhibit reproductive hormones (LH and FSH), hence acting as a non-hormonal form of contraception in the postpartum period. For LAM to be effective:
- Baby must be exclusively breastfed (no formula or solids).
- Feeding occurs at least every 4 hours during the day and every 6 hours at night.
- No return of menstruation.
This only works for the first 6 months after having a baby; its effectiveness declines as feeding patterns change. Many experts advise against this method if you use a breast pump too, as it is felt to make it less effective.
| Advantages | Disadvantages |
|---|---|
| 99.5% effective with perfect use.* | Becomes unreliable 6 months after childbirth. |
| Encourages breastfeeding which has positive effects for you and baby. Read more here. | Requires exclusively breastfeeding, and becomes unreliable if other foods/fluid is introduced into baby’s diet. |
| Can be used immediately after childbirth. | No protection against STDs. |
| No hormones, no side effects. |
*Only 2% on this method experienced an unintended pregnancy within the first year with typical use, brought down to 0.5% when used consistently and correctly. This makes it a reliable form of contraception.
Withdrawal Method
The “withdrawal method”, also known as “coitus interruptus” – where a man withdraws before ejaculation during sex – is commonly thought to be a form of non-hormonal contraception.
However, it is not recommended on its own, as it is one of the least effective contraceptive methods available. This is because sperm can be present in pre-ejaculate or pre-cum.
Interestingly, NICE clinical guidance advises that with typical use, it is 78% effective at preventing pregnancy. This is slighter better than FAMs, which is 76% effective with typical use. FAMs can be more effective if used correctly consistently, though.
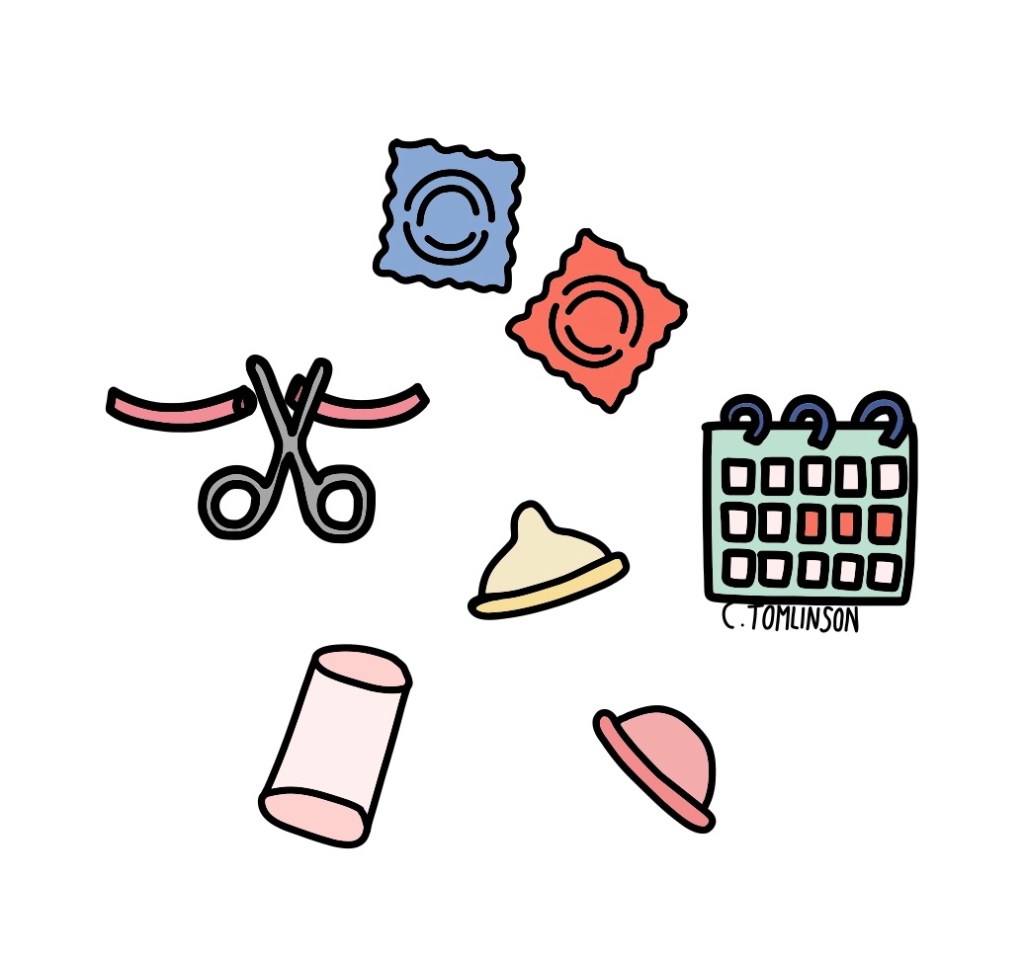
Barrier Methods
These physically block sperm from reaching the egg and are widely accessible without prescription at pharmacies, sexual health clinics, Brook Advisory Centres, or GP practices (depending on local services).
- Contraception and sexual health clinics – click here to find one near you.
- Brook Advisory centres – click here to find services available near you.
Male Condoms
Worn on the penis during intercourse, condoms provide dual protection against pregnancy and STDs. They are currently the most commonly used method of contraception in the UK. Use carefully to avoid tears – avoid oil-based lubricants which can degrade latex.
| Advantages | Disadvantages |
|---|---|
| 98% effective with perfect use, 82% with typical use.* | Forward planning required. |
| Easy to obtain and use. | They can break or slip off during sex, and oil-based products can cause them to break down, making them ineffective. |
| Protect against STDs. | Less effective at preventing pregnancy than hormonal or intrauterine contraception. |
| They’re only needed during sex. | Can reduce sensitivity and arousal during sex. |
| No hormones or hormonal side effects. | Latex allergies possible though rare; non-latex options available. |
*18% on this method experienced an unintended pregnancy within the first year with typical use, brought down to 2% with perfect use.
Female Condoms (Femidoms)
Inserted into the vagina before sex, female condoms offer an alternative to male condoms and are suitable if allergies are a concern.
| Advantages | Disadvantages |
|---|---|
| 95% effective with perfect use, 79% with typical use.* | Less effective at preventing pregnancy than hormonal or intrauterine contraception. |
| Can be used if either partner is allergic to latex. | Require forward planning and careful insertion. |
| Easy to obtain and use. | They can become dislodged or slip out during sex, or the penis may be inserted between the condom and vaginal wall making it ineffective. |
| Protect against STDs. | They can be noisy during sex. |
| Less likely to tear than the male condom. | The inner ring may cause discomfort. |
| No hormones or hormonal side effects. |
*21% on this method experienced an unintended pregnancy within the first year with typical use, brought down to 5% when used consistently and correctly.
Diaphragms and Caps
Silicone or latex domes placed at the top of the vagina (over the opening of the cervix) before sex. Cervical caps are smaller than diaphragms. They’re often used with spermicides which act as a further barrier by immobilising or killing sperm.
| Advantages | Disadvantages |
|---|---|
| Can be inserted up to 3 hours before sex. | Less effective* at preventing pregnancy than hormonal or intrauterine contraception. |
| No hormones or hormonal side effects. | Require forward planning. |
| Can’t be used until 6 weeks after childbirth, or for 6 weeks following a termination of pregnancy during the second trimester. | |
| May not reduce STD risk. NOTE – spermicides can increase infection risk, so should be avoided in people at higher risk of STDs. | |
| Must be left in place for 6 hours after sex. | |
| Sizing needs to be re-checked after weight changes of 3kg or more, and after pregnancy. | |
| Caps are less effective in women who have had children before, due to changes that occur in the cervix with childbirth. |
*Diaphragm + spermicide – 12% on this method experienced an unintended pregnancy within the first year with typical use (making them 88% effective with typical use), brought down to 6% when used consistently and correctly (94% effective with perfect use).
Cervical cap + spermicide in women who have had children – 24% on this method experienced an unintended pregnancy within the first year with typical use (making them 76% effective with typical use), brought down to 20% when used consistently and correctly (80% effective with perfect use).
Cervical cap + spermicide in women who haven’t had children – 12% on this method experienced an unintended pregnancy within the first year with typical use (making them 88% effective with typical use), brought down to 9% when used consistently and correctly (91% effective with perfect use).
Sterilisation
Permanent surgical contraception suitable for those certain they do not want future pregnancies. If you’re thinking about sterilisation as a form of contraception, make an appointment with your GP or sexual health clinic to discuss whether this is suitable for you.
Vasectomy – Male Sterilisation
Also known as getting “the snip“, this is a minor procedure performed under local anaesthetic with quick recovery. It involves cutting the Vas deferens – the tubes that transport sperm from the testicles into ejaculate and pre-ejaculate.
The procedure is quick (around 30 minutes), usually performed as an outpatient, and you can usually return to work after 24 hours.
It is very effective, with a success rate of over 99%. It is considered permanent; it can sometimes be possible to have it reversed, but this is not available on the NHS, and isn’t always successful. It is therefore only suitable for people who do not wish to have any further children.
| Advantages | Disadvantages |
|---|---|
| Very effective (>99%). | Requires a surgical procedure under local anaesthetic. |
| Permanent contraception. | Risk of surgical complications – infection, bleeding, chronic pain, failure of procedure. |
| No long-term effect on sexual performance or enjoyment. | Alternate contraception is required until a semen test confirms your semen is sperm-free (usually performed around 3 months after the procedure). |
| Not easily reversible, and people may regret having the procedure if they decide they want children later. | |
| No protection against STDs. | |
| Some studies have suggested it is linked to a higher risk of prostate cancer, though evidence is not conclusive and is felt unlikely to be directly caused by vasectomies. |
Tubal ligation – Female Sterilisation
This is where the fallopian tubes – the tubes that connect the ovaries to the womb – are blocked, to prevent egg fertilisation. It is more than 99% effective at preventing pregnancy. It does not affect your hormones or your womb, so you will still get periods.
Performed under general anaesthetic, usually via keyhole surgery (laparoscopy). Recovery times are longer due it being under a general anaesthetic, and you’ll need around a week off work.
| Advantages | Disadvantages |
|---|---|
| Very effective (>99%). | Requires a surgical procedure under general anaesthetic – there are more risks associated with this, and a longer recovery time. Click here to read more. |
| Permanent contraception. | Not easily reversible, and people may regret having the procedure if they decide they want children later. |
| No protection against STDs. | |
| The procedure can fail, and if it does, there’s a higher risk of ectopic pregnancy (where the pregnancy occurs outside of the womb). | |
| Risk of surgical complications – damage to other organs, blood clots, wound infection. | |
| Evidence suggests there is an increased risk of worsening menstrual symptoms and of subsequent hysterectomy (removal of the womb), though there is no evidence that directly links this to female sterilisation as the cause. |
In Summary
Non-hormonal contraception offers a range of effective options for those seeking to prevent pregnancy without hormones – whether due to personal preference, medical reasons, or side effects. Understanding how these options work, their effectiveness, and potential drawbacks can help you make informed choices about your reproductive health.
Not sure which type of contraception is best for you? Book in to see your GP to discuss which method is best suited to your individual needs. But to help you, here is a table summarising the above:

Further Information
For more advice on different contraceptive methods available: https://www.nhs.uk/contraception/
https://www.bpas.org/more-services-information/contraception/
Brook Advisory Centres, for sexual health advice for young people: https://www.brook.org.uk
For UK NICE guidelines for up-to-date clinical guidance:

Leave a comment