Endometriosis is one of the most common gynaecological conditions, affecting around 10% of people assigned female at birth who are of reproductive age globally. This equates to around 190 million people between the ages of 15-49, and 1.5 million within the UK alone.
This blog post explores endometriosis, it’s diagnosis and treatment options, and highlights 2 promising studies that may revolutionise care: the DETECT study focusing on diagnostic imaging and the EPiC trial exploring a novel treatment option.
What Is Endometriosis, and How Does It Present?
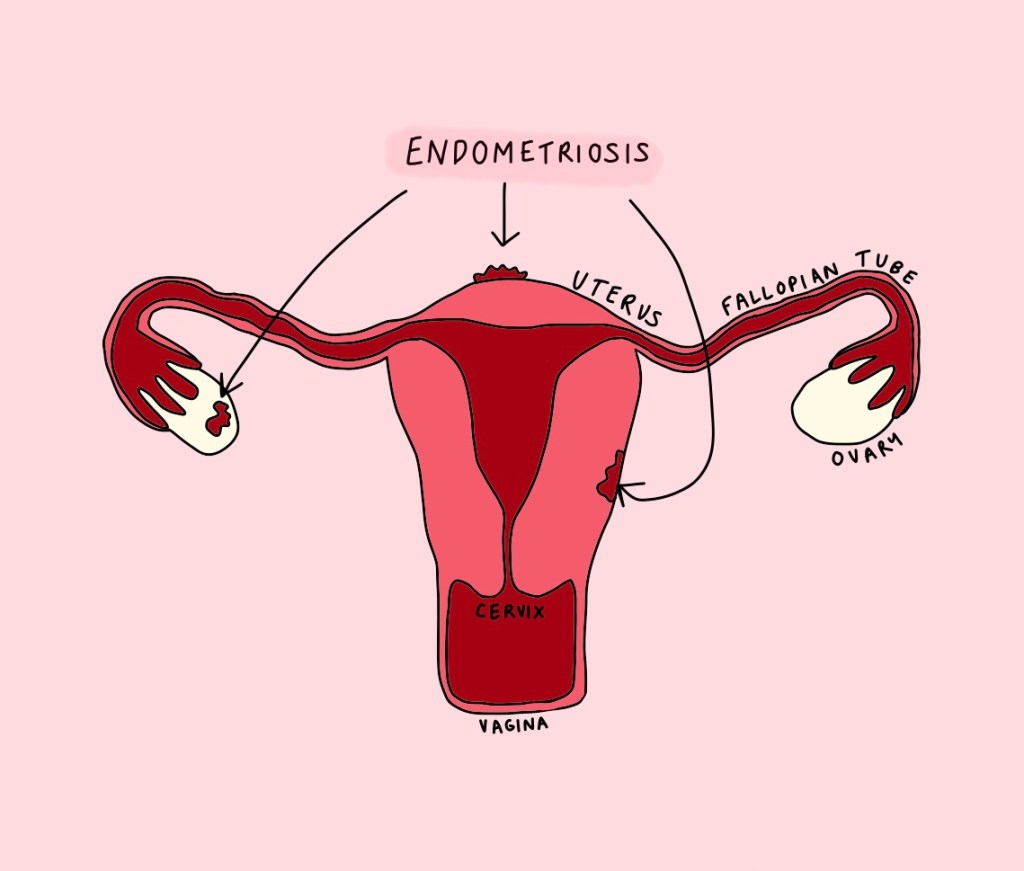
Endometriosis occurs when endometrial tissue, the tissue from the lining of the uterus (womb), grows outside of it – commonly in the ovaries, fallopian tubes, and pelvis. Currently there is no cure, and treatment is primarily focused on symptom control.
It is characterised by profound lower abdominal and pelvic pain during menstruation (periods), sexual intercourse or bowel movements.
Other symptoms include bloating, fatigue, and infertility. Additionally, individuals with endometriosis often experience higher rates of anxiety and depression. Up to 20% may have a concurrent chronic pain condition such as fibromyalgia or migraines.
What Causes It?
The exact cause of endometriosis remains unknown. However, it is believed that endometrial tissue is carried up into the pelvis during a period, known as “retrograde menstruation”. There’s currently no known way to prevent it.
How Is It Diagnosed, and Why Does It Take So Long To Be Diagnosed?
Diagnosis typically involves several steps:
- Seeing a Gynaecologist: The doctor will ask about symptoms and perform a pelvic examination.
- Examination may show a tender and enlarged mass over the ovaries, which suggests a diagnosis of an endometrioma (a cyst within the ovaries due to endometrial tissue growing there).
- Imaging: usually a transvaginal and abdominal ultrasound.
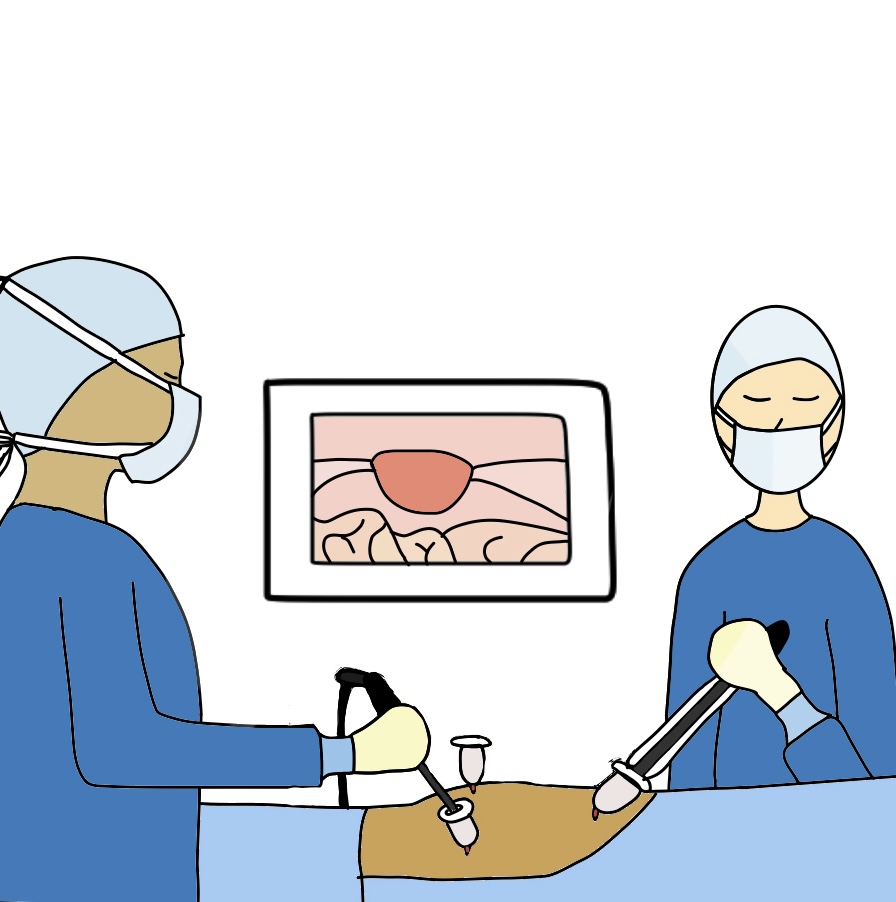
- Definitive diagnosis: Achieved by diagnostic laparoscopy (keyhole surgery) – a minimally invasive surgery that looks inside the abdomen and pelvis. If endometrial tissue is visualised, it can be removed.
Endometriosis often goes undiagnosed and misdiagnosed for many years; diagnosis on average takes 7.5 years from the onset of symptoms.
Why Does Diagnosis Take So Long?
- Symptom variability: symptoms can present similarly to other gynaecological conditions e.g., fibroids, so these conditions will likely be investigated and ruled out first (as it is generally easier to do so). Endometriosis is also more likely to be misdiagnosed as a result.
- Invasive procedure required for definitive diagnosis: This may deter patients due to the potential risks associated with surgery, and healthcare practitioners tend towards treating suspected endometriosis empirically before a definitive diagnosis is made.
- Reliability of current investigations: Current tests can vary in effectiveness depending on the location of endometrial tissue and how extensive the disease is, as well as the experience and expertise of the healthcare provider.
- Ultrasound is very good at picking up endometriomas within the ovaries, but has a high false-negative rate* for peritoneal endometriosis**.
- Laparoscopic visual diagnosis can also be unreliable as endometrial tissue varies significantly in colour, size, shape, and location from person to person. This is why tissue samples need to be sent to the lab for analysis too (though this can be hard if there are no obvious areas of endometrial tissue to sample).
- Lack of awareness: Both healthcare practitioners and the public often lack awareness about endometriosis, leading to the common misconception that periods are supposed to be painful***.
- Societal stigma: Stigma surrounding discussing women’s health in society can delay people presenting to their healthcare practitioner.

*False-negative rate = how likely it is that a test suggests a person doesn’t have a condition when they actually do have it. The higher this is, the more likely it is that a condition will go missed.
**Peritoneal endometriosis – where endometrial tissue is within the peritoneum, the peritoneum being the lining of the abdomen + pelvis, surrounding the organs within these areas. This is the earliest stage of the disease (see image to the left).
Pain that stops you from doing your normal activities for several days a month is NOT normal. Mild pain during your period can be normal, and typically starts 1-2 days before your period and lasts for a few days. Period pain tends to be worse when you are starting your periods and should improve as you get a bit older, and as your cycles become more regular.
What Is The Impact of a Delayed Diagnosis of Endometriosis?
A delayed diagnosis in endometriosis can have a significant impact on a person’s life, leading potentially to prolonged pain and suffering, mental health challenges, disease progression resulting in fertility issues that could’ve been mitigated by earlier treatment, difficulties in interpersonal relationships, and loss of trust in healthcare providers.
Delayed diagnoses impose a financial burden on the NHS, costing around 8.2 billion pounds a year in working time and treatment costs.
How Might The Way We Diagnose Endometriosis Change In The Future?
Recent advancements suggest that the ongoing DETECT study at the University of Oxford could revolutionise the way that endometriosis is diagnosed. Preliminary data released in March 2024 suggests that a new imaging agent called 99mTc-maraciclatide can accurately visualise superficial peritoneal endometriosis – accounting for around 80% of diagnoses – potentially eliminating the need for surgical confirmation.
99mTc-maraciclatide is a a special type of contrast that binds to a protein (αvβ3) essential for new blood vessel formation, which is needed for endometrial tissue growth. This tracer shows up on SPECT- CT imaging, allows for identification of areas of endometrial tissue.
SPECT-CT = a type of CT scan (computerised tomography) using which uses a radioactive tracer.
How Does This Study Work?
The study is still ongoing at present and is looking at 25 people with known or suspected endometriosis who are awaiting laparoscopy. Prior to surgery they undergo SPECT-CT imaging with 99mTc-maraciclatide as a tracer to identify areas of endometrial tissue.
During laparoscopy, tissue samples from areas where endometrial tissue is visualised directly are taken and sent to the lab. The samples from the lab are then compared with the imaging with 99mTc-maraciclatide to assess accuracy.
Results from the preliminary data looks promising; the results of the full study are expected later this year.
If successful, this could help speed up diagnosis of early-stage disease (thus reducing diagnostic delay and allowing for earlier intervention), and reduce the risks associated with diagnostic laparoscopy. It will also aid in the detection of disease in areas that are not easily seen during surgery (e.g., in the lungs – albeit rare), and may help to reduce the healthcare burden (as a quick 20-minute scan may lessen the need for multiple visits to a healthcare practitioner, various investigations and invasive surgery).
How Is Endometriosis Treated Now?
There are non-surgical and surgical treatments for endometriosis:
- Non-surgical treatments: Primarily involve hormonal therapies (endometrial tissue is affected by hormones in the same way as endometrial tissue inside the womb; hormonal treatment acts to slow down the growth of endometrial tissue) and analgesia for pain relief.
- Surgical options: These include laparoscopic removal of endometrial tissue and endometriomas. In some women, hysterectomy (removal of the uterus) may be considered.

How Might The Treatment of Endometriosis Change In The Future?
In another exciting development, researchers at the University of Edinburgh have identified Dichloroacetate (DCA) – a drug currently used to treat metabolic conditions in children – as a potential treatment for endometriosis-related pain based on preclinical data from the EPiC trial. This is particularly significant, as there have been no new treatments for endometriosis in the past 40 years.
This trial marks the first investigation into the efficacy of DCA in the treatment of endometriosis-related pain and aimed to assess the feasibility of recruitment and retention rates for such a trial (which could potentially inform a future larger scale trial into the use of DCA for this purpose).
It involved 30 people with surgically confirmed stage 1-2 endometriosis receiving oral DCA for 12 weeks, and then being followed up by a phone call 4 weeks post-treatment to assess symptom changes.
Results indicate that cells within endometrial tissue exhibit altered metabolism compared to those without the condition; these cells produce more lactate which is similar to the behaviour of cancer cells.
- Higher levels of lactate in cancer cells promotes the formation of new blood vessels, which in turn drives further spread of cells into tissues; it’s believed that higher levels of lactate drive the propagation of endometrial tissue in the same way.
DCA treatment seems to normalise this metabolism, reducing lactate levels and thus slowing down the abnormal growth of endometrial tissue.
A non-hormonal treatment such as DCA would help mitigate side effects associated with current hormonal therapies (including mood changes and weight gain), as well as maintaining fertility whilst on the treatment (as current hormonal treatments also act as contraception) allowing for more personalised treatment plans.
A Personal Story Shared; Annabel’s Experience of The Difficulties She faced in obtaining a diagnosis
Annabel is a 20-year-old who was initially diagnosed with endometriosis after having an Ultrasound scan. She later had a diagnostic laparoscopy which failed to show any active disease at the time. This is her experience:
“I first went to my GP with symptoms of irregular and heavy periods, and constant pelvic pain aged 18. The first consultation was over the phone, and I was offered the copper coil to help with my symptoms, as I have previously had a negative reaction to hormonal treatments. The copper coil exacerbated my initial symptoms and one on occasion landed me in hospital, as the bleeding was so heavy that I dropped my blood pressure. While in hospital I had an Ultrasound scan which was normal; I wasn’t given an answer for my symptoms and was discharged with advice to have my copper coil (IUD) replaced by the Mirena coil (IUS).
After my symptoms continued to worsen and resulted in another A&E attendance, I was referred to Gynaecology, where I was seen after 10 months. They offered a repeat Ultrasound and a laparoscopy. The Ultrasound this time showed a 4.2cm endometrioma on my right ovary.
Whilst waiting to see the Gynaecologist I had to attend the GP practice multiple times due to my symptoms. On one occasion I was also turned away from A&E when my symptoms became unbearable and told there was nothing they could do for a “heavy period”.
I then underwent a laparoscopy; on the day I attended the unit I felt dismissed because of my age, overhearing staff making remarks that I was “too young to be having a laparoscopy”. Despite this being a “minimally invasive” procedure, when I came round in the recovery bay I was in agony – I was then questioned by staff as to why I was crying, which left me embarrassed for feeling this way.
I was subsequently told by the Gynaecologist that I didn’t have endometriosis, despite having previously been told after having an Ultrasound 2 months prior that I did have it, and it being documented in my discharge letter that I had adhesions around my appendix and in my pelvis which is a sign of endometriosis too.
I was then discharged without a follow up appointment and left feeling very confused about my diagnosis and treatment going forwards.
This whole experience was mentally challenging, and I felt no one was taking me seriously. At 19, I was having to argue with Senior Consultants about symptoms, as I kept being told I would “grow out” of them. I still haven’t grown out of my symptoms, nor are they getting any better, but I am trying to manage them as best I can by living healthily and with pain relief.
If a CT scan was available to me, I would’ve opted for this, as it would’ve likely given me the answer I’m looking for in a less painful way. I am also hopeful that more non-hormonal treatments will be available in the future, as the options for me are very much limited at the moment.
Whilst my experience with diagnosis and treatment was poor and everyone’s experience is different, the research and time being invested into this prevalent disease fills me with confidence that other women and girls will be taken seriously and diagnosed in a more efficient and less invasive way.”
In Summary.
While endometriosis remains a challenging condition to diagnose and treat, research advancements offer hope for improved diagnosis and treatment.
Remember, severe period pain that disrupts your daily life is not normal. If you suspect that you may have endometriosis, please speak to your healthcare practitioner, and keep a detailed record of your symptoms to help aid in diagnosis.
Do you think 99mTc-maraciclatide and DCA could bring about the change we need to see in diagnosing and treating endometriosis? I’d love to hear your thoughts – please leave a comment down below!
Learn More About Endometriosis Below:
https://www.endometriosis-uk.org
https://www.nhs.uk/conditions/endometriosis/
References:
All references are hyperlinked in this blog post – click on highlighted words for more.

Leave a reply to Charlotte Cancel reply