The menopause – we’ve all heard of it, and it’s an inevitability for all women at some stage in their life. When we think of the menopause, what do we think of? Chances are the first thoughts that pop into our head aren’t entirely positive ones – think brain fog, mood swings, and more.
But, what actually is the menopause? And do we have really have to just “grin and bear it”? The answer is no. In a sense, menopause is medical, and it is more than a ‘life stage’.
For our first article as part of Women’s Health Week, let’s deep dive into the menopause. What does this term actually mean? What symptoms may you experience? And what can doctor do to help make things more manageable?
This article is designed to help raise awareness and should not be taken as definitive medical advice. Medicine and healthcare are highly individual – always consult your own doctor before making health decisions.
Contents
- What is the menopause?
- The hormones behind it all
- Common symptoms: What to expect
- Menopause diagnosis
- Let’s talk about HRT
- Non-hormonal menopause management
- Sex and the menopause
- Contraception and the menopause
- Support and resources
- What about workplace support?
- Menopause isn’t the end, it’s a new chapter
What Is The Menopause?
The menopause is a biological stage in a woman’s life where menstruation (periods) stop altogether, due to the ovaries stopping working. It is diagnosed clinically 12 months after your final period. It usually occurs between the ages of 45 and 55, with the average age in the UK being 51 years old.
It occurs naturally around middle age, although can occur earlier due to:
- Hysterectomy (surgical removal of the womb)
- Oophorectomy (surgical removal of the ovaries)
- Certain cancer treatments like chemotherapy
- Genetic reasons
Leading up to the final period, there is often a phase called the ‘perimenopause‘, ‘menopausal transition‘, or ‘climacteric‘. During this time, there is a fluctuation in the function of the ovaries. You may start to develop symptoms in this phase (which can later improve for a time!), and it can last several months – years.
Early Menopause, Premature Menopause, And Premature Ovarian Insufficiency
Early menopause occurs when the ovaries stop functioning between the ages of 40-45 years old.
Premature ovarian insufficiency (POI) is where the ovaries are not working properly, and this occurs before the age of 40. Sometimes this loss of function is temporary (though this possibility is small), but other times, there is an irreversible loss of ovarian function, referred to as premature menopause. With POI, you may still have irregular or occasional periods for years, and it may still be possible to get pregnant. With premature menopause, you will not be able to become pregnant.
Early/premature menopause can happen naturally, or as the result of medical treatments like chemotherapy, radiotherapy, or surgery.
The Hormones Behind It All
The ovaries contain lots of ovarian follicles (fluid-filled sacs) that are responsible for producing two important hormones – oestrogen and progesterone. These hormones play a pivotal part in regulating the menstrual cycle:
- Oestrogen is responsible for the release of an egg cell from ovarian follicles (ovulation) once during each menstrual cycle, which may be fertilised by sperm cells if there is change of pregnancy.
- After the egg cell is released from the ovary, progesterone levels increase too, which helps prepare the body for pregnancy by thickening the lining of the womb (endometrium).
- If the egg isn’t fertilised, it is passed out of the body along with the womb lining during menstruation.
In the menopause, the number of ovarian follicles significantly declines, so the levels of oestrogen and progesterone decrease and the ovaries stop releasing egg cells. In response, the brain ramps up its signals to the ovaries by increasing levels of the hormones FSH (follicle-stimulating hormone) and LH (luteinising hormone) released by the pituitary gland.
Increasing levels of FSH/LH would typically increase oestrogen and progesterone levels in pre-menopausal women. However, in menopausal women, with fewer ovarian follicles available to produce hormones, the ovaries can’t respond in the same way. This hormonal disruption is what leads to many of the symptoms of menopause.
Common Symptoms: What To Expect
- Menstrual changes – periods may change in length, frequency, and amount of blood loss.
- Vasomotor symptoms, a.k.a. hot flushes and night sweats – a sudden feeling of heat in the body, typically lasting a few minutes at a time. Common triggers include spicy foods or alcohol. These are the most common symptoms of the menopause, occurring in 75% of women.
- Urogenital symptoms – vaginal dryness and irritation (which can cause discomfort during sex, known as dyspareunia), pain on passing urine (dysuria), increased frequency of needing to pass urine, urinary incontinence, and recurrent urinary tract infections (UTIs).
- Generalised aches and pains
- Weight gain
- Mood changes – such as low mood, irritability, mood swings. Some studies suggest there is an increased susceptibility to mental health conditions such as anxiety and depression, too.
- Loss of libido
- Sleep disturbance – this may be due to vasomotor symptoms, or due to mood changes or insomnia.
- Brittle nails
- Thinning of skin
- Hair loss
Why Does The Menopause Increase The Risk of Osteoporosis and Heart Disease?
Oestrogen plays a role in bone breakdown and rebuilding. In the menopause, bones break down faster than it is rebuilt, leading to a gradual loss in bone density. This increases the risk of developing osteoporosis, where the bones become weaker and are more likely to break.
Oestrogen also reduces the levels of LDL cholesterol, or “bad” cholesterol, in your blood, whilst increasing HDL cholesterol, “good” cholesterol. Lower oestrogen levels therefore increase the risk of cholesterol building up in the arteries, in turn narrowing them, subsequently increasing the risk of heart attacks and strokes.
Menopause Diagnosis
A diagnosis of perimenopause is suspected if there is a change in the pattern of a woman’s menstrual periods +/- vasomotor symptoms. A diagnosis of menopause is made 12 months after the final period.
Bloods tests are not usually needed to diagnose the menopause in women aged over 45 years old, with typical menopausal symptoms.
If your symptoms are unusual, or you are aged under 45, your doctor may consider a blood test to check the level of FSH in your blood. This test will be repeated after 4-6 weeks.
Let’s Talk About HRT
While not everyone needs treatment, for many women, symptoms can become disruptive. Thankfully, there are options – especially hormone replacement therapy (HRT), which can be tailored to your needs and medical history.
Not only is HRT beneficial for symptom management in the menopause, but it helps to reduce the risk of osteoporosis and maintain muscle strength.
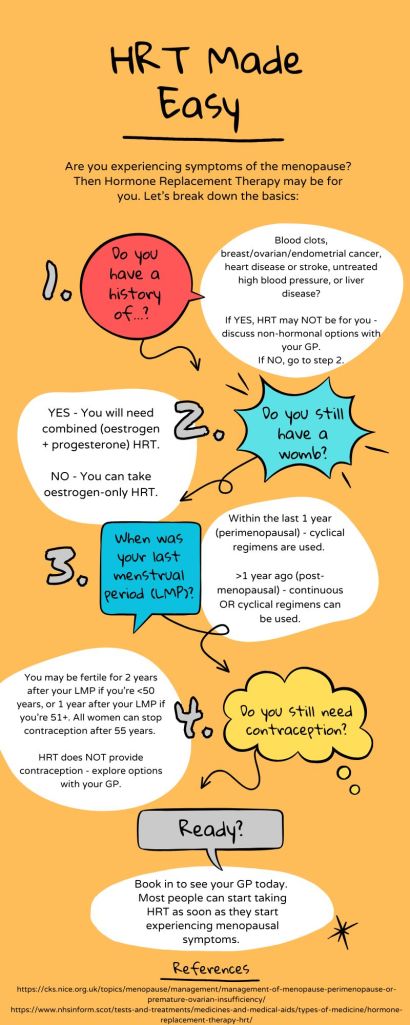
HRT Types
- Combined (oestrogen + progesterone) – this type is prescribed for women who still have a womb.
- Oestrogen-only – this type can be prescribed for women who have had a hysterectomy.
- If you were to take oestrogen-only HRT when you still have a womb, the womb lining would continue to thicken, increasing the risk of endometrial cancer.
HRT Regimens
- Cyclical regimens – also known as sequential HRT. It involves taking oestrogen continuously, and progesterone only for part of the month (14 days) or for 14 days every 3 months as part of a 3-monthly regimen. After you finish taking the progesterone you will have a period-like bleed (withdrawal bleed). This is commonly used for women still having periods.
- Continuous regimens – oestrogen and progesterone are taken all the time, so there will be no withdrawal bleed. This is commonly used in post-menopausal women.
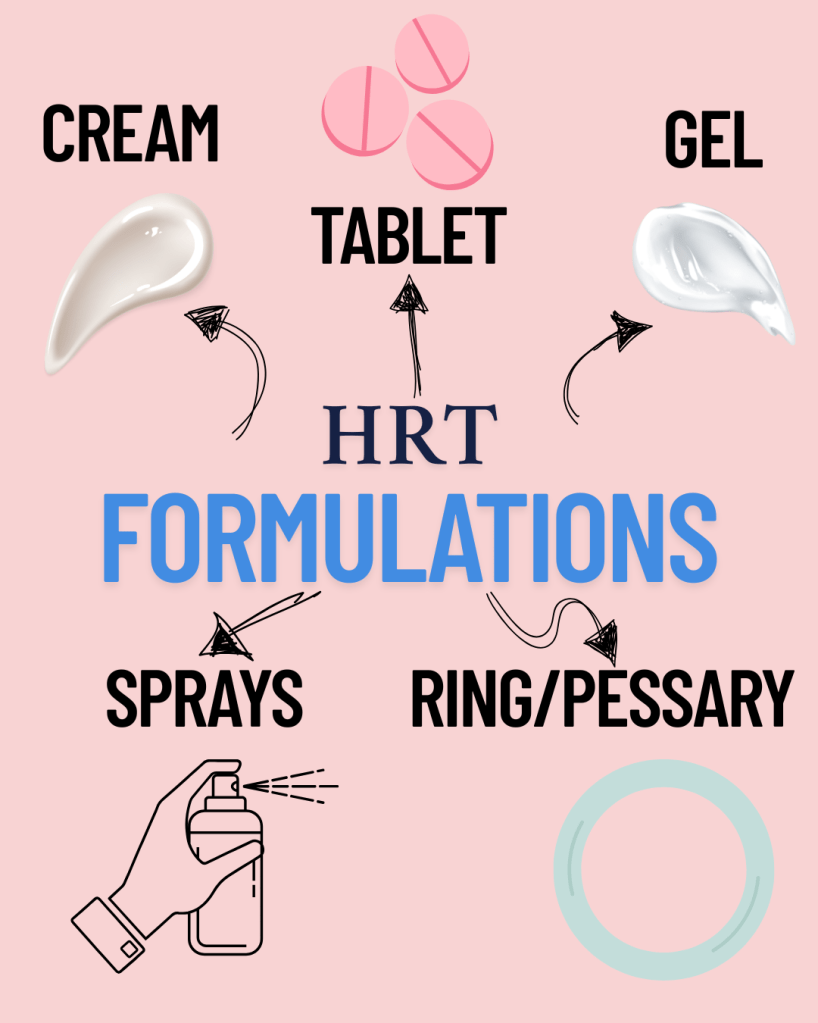
HRT Formulations
Your Personalised HRT Pathway: A Quick Guide
HRT prescribing can be confusing for both patients and practitioners alike. Here is a simple flowchart to help break it down:
Risks and Side Effects of HRT
- Oestrogen-related side effects: fluid retention, bloating, breast tenderness, reflux, nausea, headaches.
- Progesterone-related side effects: headaches, mood swings, fluid retention, breast tenderness, acne.
- Irregular bleeding is a common side effect within the first 3 months of starting HRT, or up 6 to months if continuous combined HRT.
- If bleeding occurs after 6 months, if the pattern of bleeding changes or becomes heavier, then you should see your doctor to rule out another cause of irregular bleeding.
- Blood clots
- Oral HRT (tablets) is associated with a small increased risk of venous thromboembolism (VTE).
- Transdermal HRT (patches, gels, sprays) does not carry this increased clot risk and is the safer option, especially in women at higher baseline risk (e.g. BMI >30, smokers, family history of VTE).
- Strokes
- Oral HRT slightly increases the risk.
- Breast Cancer – the risk increases the longer you take it, and the older you are.
- Combined HRT (oestrogen + progesterone) may slightly increase the risk of breast cancer, particularly with long-term use (>5 years).
- Oestrogen-only HRT has a much lower associated risk.
Discuss your individual risk factors with your GP. For many women, the benefits of HRT outweigh the risks, especially if started before the age of 60 or within 10 years of menopause onset.
Non-hormonal Menopause Management
Not everyone wants – or is suitable – for HRT. Fortunately, there are a range of non-hormonal options that can help manage symptoms:
- Exercise: Weight-bearing exercise helps protect against bone loss and boosts mood.
- Diet: A balanced diet with plenty of calcium and vitamin D supports bone health.
- Sleep hygiene: Regular routines and screen time limits can improve sleep.
- Stress reduction: Yoga, mindfulness, and CBT can help for mood symptoms.
- SSRIs/SNRIs: Certain antidepressants (e.g., venlafaxine) can help reduce hot flushes.
- Clonidine: A blood pressure medication also used to treat hot flushes.
- Gabapentin: Sometimes used off-label to reduce night sweats and aid sleep.
- Non-hormonal vaginal moisturisers or lubricants can be helpful for urogenital symptoms e.g. vaginal dryness. In some cases, topical vaginal oestrogen may be prescribed, even if systemic HRT isn’t.
If the above treatments don’t improve your symptoms, you may be referred to a healthcare professional with expertise in the menopause.
Sex and the Menopause
Menopause can affect your sex life – both physically and emotionally. Common changes include:
- Vaginal dryness or tightness (causing pain during sex)
- Lower libido (reduced interest in sex)
- Changes in partner dynamics or confidence
These are normal, but they are not untreatable. Options include:
- Vaginal oestrogen pessary/creams/rings: These act locally to restore vaginal lining and reduce dryness without systemic hormone absorption.
- Moisturisers and lubricants: Available over the counter.
- Testosterone therapy: Not yet licensed for women in the UK but sometimes prescribed off-label to improve libido in postmenopausal women, especially when HRT hasn’t helped/can’t be taken.
Talking openly with your partner and GP can help navigate these changes. Intimacy doesn’t have to stop – it may just need to evolve.
Contraception During The Menopause
NICE clinical guidance advises that:
“a woman is potentially fertile for 2 years after her last menstrual period if she is younger than 50 years of age, and for 1 year if she is over 50 years of age.”
HRT is NOT contraception, so additional contraception may be needed alongside your HRT. The exception to this is the Mirena coil, which can be used to provide the progesterone element of HRT and for contraception. All women can generally stop contraception after 55 years of age.
Support And Resources
NHS Menopause Guide – nhs.uk/conditions/menopause
The Balance App by Dr Louise Newson – an app allowing you to track your symptoms, seek more advice, and access community support, founded by GP and menopause specialist Dr Louise Newson. https://www.balance-menopause.com/balance-app/
Women’s Health Concern – provides independent advice, with multiple factsheets specifically relating to the menopause (from nutrition in the menopause, to exercise, and more). www.womens-health-concern.org
Menopause Matters – a website providing up-to-date information about the menopause, and treatment options. www.menopausematters.co.uk
The Daisy Network – a charity supporting women with premature ovarian insufficiency (menopause before 40). https://www.daisynetwork.org
Menopause cafés – informal spaces to meet and talk about menopause, held all across the UK. https://www.menopausecafe.net
What About Workplace Support?
Menopause can have a significant impact on a woman’s working life. It is important to remember though that menopause is normal, and that support should be available in the workplace, too.
Companies are increasingly adopting menopause-friendly policies, such as:
- Flexible work hours
- Workplace adaptations – e.g. a lighter uniform if you are experiencing hot flushes, or having access to a fan
- Menopause awareness training
If you’re struggling, don’t hesitate to speak to HR or occupational health.
Menopause Isn’t The End – It’s A New Chapter
Though menopause is a universal experience, it has often been shrouded in silence or shame. But what if we flipped the narrative?
Many women describe life post-menopause as liberating – free from periods, contraception worries, or hormonal mood swings. With the right support, this phase can be one of power, stability, and clarity.
Whether you’re experiencing symptoms, supporting someone who is, or just learning more – speak up, ask questions, and don’t settle for suffering in silence.
Have your or someone your know experienced symptoms of the menopause or perimenopause? What support made the biggest difference? What do you think needs to change in how society or the healthcare system talks about and supports women through this stage of life?
I’d love to hear from you! Please leave a comment down below.

Leave a reply to Joy Kean Cancel reply